Dr. Munish Goyal comes to us all the way from downtown DC, where at the Georgetown University School of Medicine he acts as Director of Emergency Intensive Care and Associate Program Director for the Pulm/Critical Care Fellowship. Using his positions in both the Emergency Department and the Pulmonary and Critical Care department, he has been able to revolutionize the way cardiac arrests are treated – implementing protocols that transition care from ED to ICU to discharge. In today’s talk he takes us through some common ACLS scenarios and then asks simple questions with some unexpected answers…… In just 57 minutes he just might make you question the way you handle your next crashing patient!!
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Handling your next code, The Munish Goyal Method:
Chapter 1: Epinephrine
- Used for α effects with the goals
- Afterload → ↑ Diastolic Pressure → ↑ Coronary Perfusion Pressure (CPP)
- CPP = Diastolic Pressure – Right Atrial Pressure
- ROSC has been achieved ONLY when CPP > 15mmHg
- At the expense of β effects
- ↑ HR → ↑ Contractility → ↑ Myocardial O2 Demand
- ↓ Microvascular Perfusion (brain, lungs, etc.)
- 1mg vs. 5mg Epi?
- There is NO change to outcome!!
- Same D/C rate, same Neurological Outcome
- In fact, studies show NO benefit at ANY dose of Epi!!
- “May help, probably doesn’t hurt”
- Afterload → ↑ Diastolic Pressure → ↑ Coronary Perfusion Pressure (CPP)
TAKE AWAY #1: Epinephrine is a great drug to assist ROSC, however DO NOT use at the EXPENSE of a working organ. Don’t take away from great CPR just to get access for a drug that might not really do anything!!
Chapter 2: Electricity!
- 1) Time to shock is directly correlated with outcome
- a) <2 mins = 2/3 achieve ROSC with 39% survival
- b) >2 mins = 1/2 achieve ROSC with 22% survival
TAKE AWAY #2: Shock the unstable rhythm first, ask questions later!
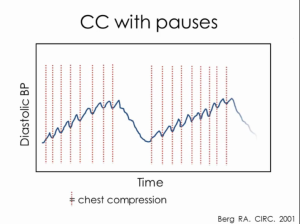
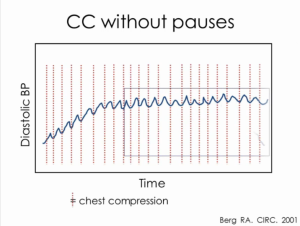
Chapter 3: Chest Compressions
1) Any pause = ↓ CPP
TAKE AWAY #3: Minimize interruptions, even at the expense of lines or tubes
Chapter 4: Airway and Oxygenation
- No increase in survival with early intubation
- Average PAUSE to CPR: 46.5 seconds (please see above!)
- Hyperventilation is common and causes ↑ Intrathoracic Pressure → ↓ CPP → ↓ ROSC
- Hyperoxia is just as bad as Hypoxia!
- a) ↑ Neural Cell Injury
- b) ↓ Neurological Outcomes and need for rehab
- c) ↑ Mortality!!
TAKE AWAY #4: Ventilate with the MINIMUM breaths, FiO2 and PEEP!!
Chapter 5: Epi + Vaso + Steroids?!?
- Appears to lead to better outcomes:
- ↑ Diastolic Pressure
- ↓ Inflammatory Markers
- ↑ Cerebral Perfusion Pressure
- Taken together there ↑ survival to D/C and Improved Neurological Outcome
- Unclear whether it is the steroids or vasopressin (or both together) that may improve outcomes
TAKE AWAY #5: Jury’s still out, but Epi/Vaso/Methylpred may be the next big discovery!!
Chapter 6: Hypothermia
- Proven only in VF and VT (Not Asytole or PEA)
- Proven only out of hospital arrests (not floor arrests)
- Like all of medicine: Timing is EVERYTHING
- Any delay = ↓ survival
- At 8 hrs there is no longer a benefit
TAKE AWAY #6: You won’t be punished for cooling a patient, but you may if you don’t.
Suggested Reading
- Olasveengen TM, Sunde K, Brunborg C, Thowsen J, Steen PA, Wik L. Intravenous drug administration during out-of-hospital cardiac arrest: a randomized trial. JAMA. 2009;302:2222–2229.
- Mentzelopoulos, S. D., Malachias, S., Chamos, C., Konstantopoulos, D., Ntaidou, T., Papastylianou, A., Kolliantzaki, I., Theodoridi, M., Ischaki, H., Makris, D., Zakynthinos, E., Zintzaras, E., Sourlas, S., Aloizos, S., & Zakynthinos, S. G. (2013). Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest: a randomized clinical trial. Journal of the American Medical Association, 310(3), 270-279.
- Berg RA, Sanders AB, Kern KB. et al. Adverse hemodynamic effects of interrupting chest compressions for rescue breathing during cardiopulmonary resuscitation for ventricular fibrillation cardiac arrest. Circulation. 2001;104:2465-2470.